The mission of The National MDS Study (ClinicalTrials.gov Identifier: NCT02775383) is to build a resource that scientists can use to learn more about a group of rare bone marrow diseases called myelodysplastic syndromes (MDS). The National MDS Study will enable scientists to conduct research that will improve the way MDS is diagnosed and how it is treated. The study will also enable scientists, patients, and their families to better understand what to expect when a patient is diagnosed with MDS. The National MDS Study is sponsored by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the National Cancer Institute (NCI).
MDS Predictive Tool
The MDS study has developed a 2-stage diagnostic classifier based on mutations in 18 genes that can be applied alone or in combination with a morphologic review to predict diagnosis of myeloid malignancy and MDS. Please click the link below to access our online predictive tool which is referenced in our Blood Advances publication (DeZern et. al., 2023).
About the National MDS Study
The National MDS Study will establish a cohort of 2,000 adults recently diagnosed with MDS and 500 adults with idiopathic cytopenia of undetermined significance (ICUS). These volunteers will donate biological specimens (like bone marrow and blood) and medical information, including details of their symptoms, how they perceive their quality of life, the treatments they receive, and what their doctor says about the severity of their illness over time. This information will be collected at pre-determined time points for the duration of the study. Study participants may be followed for life.
Participants will be enrolled in the National MDS Study at clinics in the U.S. that are part of the NCI Clinical Trials Network (NCTN) or the NCI Community Oncology Research Program (NCORP). Biological specimens will be stored at M2Gen, a wholly owned subsidiary of the Moffitt Cancer Center. Clinical data will be collected at the NCTN and NCORP centers and stored at the study’s Data Coordinating Center, The EMMES Corporation.
The primary objective of the National MDS Study is to create a comprehensive, standardized longitudinal clinical data set linked to consistently processed, well-annotated biospecimens that can be used by scientists interested in MDS research. Potential uses for this resource include: (1) identifying genetic, epigenetic and biological factors associated with initiation and progression of MDS; (2) uncovering fundamental information on the changes that occur in hematopoietic stem cells and bone marrow stroma in patients with MDS, and how this differs from what happens during normal aging; (3) discovering biomarkers of disease onset or progression, or response to therapy; (4) identifying potential targets for new therapeutic interventions; and (5) improving clinical management of MDS patients.
Why MDS?
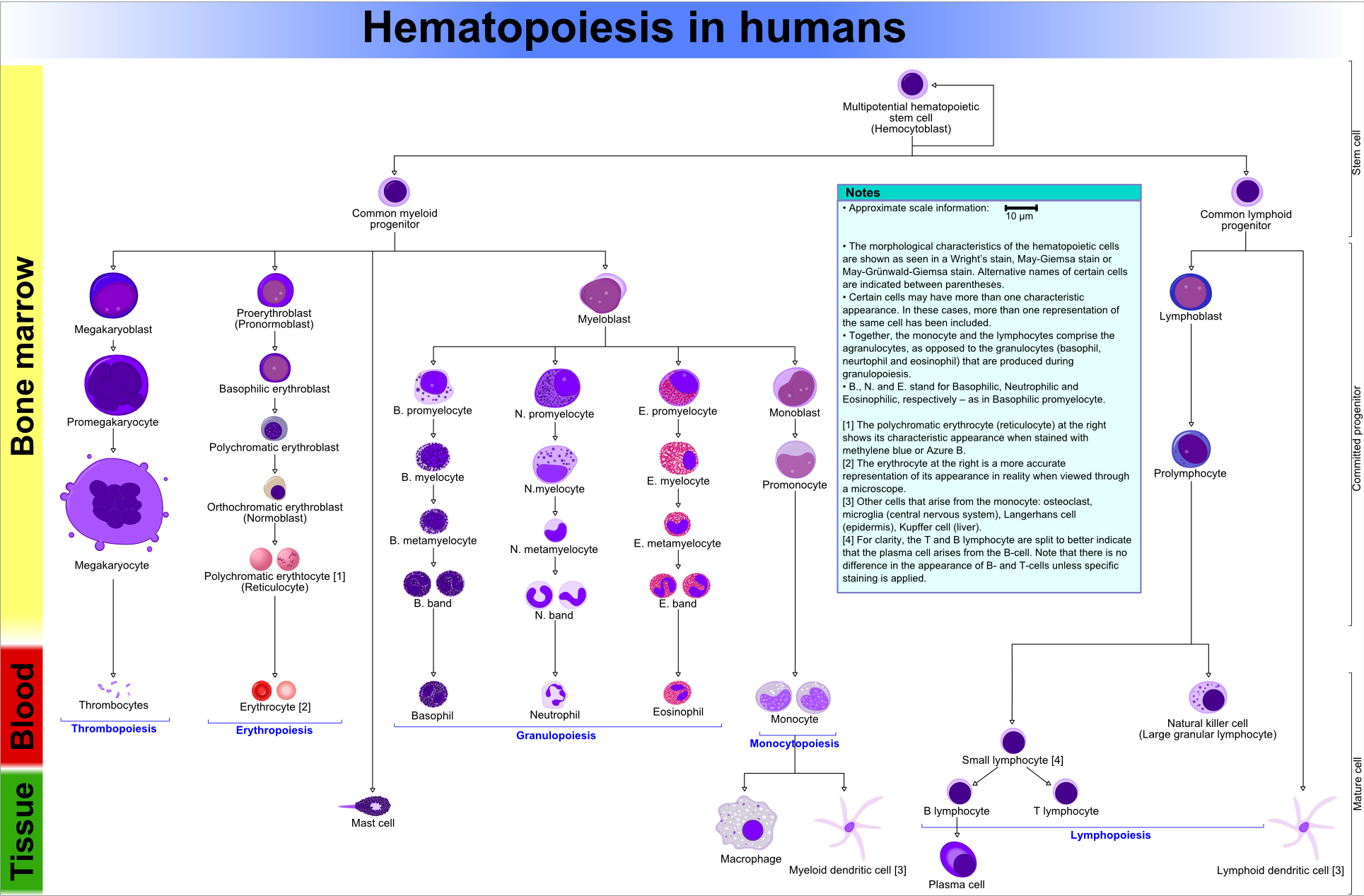
MDS are a group of a progressive bone marrow diseases characterized by failure of the bone marrow to generate normal blood cells. The bone marrow is the organ in the human body that makes blood cells that are essential for critical physiologic functions. These cells include platelets (also called thrombocytes) that make your blood clot, red blood cells (erythrocytes) that carry oxygen in your blood, and most of the white blood cells in our bodies that fight infection. For these cells to carry out their functions, they must be produced in adequate numbers and must be functioning normally. In patients with MDS, the blood cells that are produced are too few in number and they are dysfunctional.
Blood cells are formed from stem cells in the bone marrow. The diagram below illustrates this process and it shows which kinds of blood cells are ultimately affected in MDS.
Source: Wikipedia
As the diagram shows, MDS is a disease associated with cells in the myeloid lineage. When myeloid cells look abnormal under the microscope, they are called dysplastic. Thus, the name of the disease: myelodysplastic. Because MDS patients have too few or improperly functioning blood cells, their blood does not clot properly and they are at higher risk for life-threatening infections than people who don’t have MDS. In addition, about 1/3rd of patients who have MDS are at risk for developing a blood cancer called acute myeloid leukemia (AML).
MDS is diagnosed in least 10,000 people each year in the United States, and approximately 60,000 people are living with the disease in the US today. Most cases of MDS occur in people age 70 or older. About 90% of MDS patients have what is called de novo MDS, meaning the disease arises with no apparent cause. Approximately 10% of patients get MDS because of prior treatment for cancer, e.g., with chemotherapy or radiation, and are therefore said to have therapy-related MDS. A very small proportion of patients have MDS as a result of an inherited genetic condition affecting their bone marrow, such as Fanconi anemia. These patients are typically children, and the types of MDS that children get are generally different from the MDS that adults get. There are also some other bone marrow diseases, called MDS/MPD (where MPD means myeloproliferative disorders), that look a little bit like MDS but have some unique characteristics of their own. More research is required to understand the nature of MDS/MPD and how best to treat them.
MDS can be divided into high risk and low risk disease, where higher risk MDS is associated with a greater chance of death or transformation to AML. The only way to cure MDS is through a stem cell transplant. Stem cells can be obtained from many sources, including bone marrow, blood, or umbilical cord blood. Unfortunately, stem cell transplants are not possible for all MDS patients because sometimes it is difficult to find a stem cell donor, and not all patients are healthy enough to undergo the procedure. There are other drugs available to treat MDS, and although some may prolong survival by a small amount, many simply treat the symptoms of MDS and none have the potential to cure the disease. Therefore, it is very important that more research be done to develop a cure for MDS.
Should I join a clinical trial?
If you are considering joining a clinical trial such as the National MDS Natural History Study, we recommend first learning about the trial's goals and how involvement in the study may benefit you and/or society. Please remember to always consult with your physician to ensure that you meet study criteria and that your participation in the study will not negatively impact any current treatment or underlying conditions. If you are interested in additional general information about clinical trials, please click here to access a March 2023 article published in The Washington Post's personal health section, Well+Being, where MDS Study Chair, Dr.Mikkael Sekeres , offers expert advice.
